Can You Please Tell Us Again Where to Find the Drug List Am Not Finding It Did You Say Bcbscom
Nigh patients with Blue Cantankerous NC health insurance also have a medication plan to cover the medications they get at their pharmacy. Each medication programme comes with a list (or formulary) that shows you what medications are covered.
Are your patient'due south prescription medications covered?
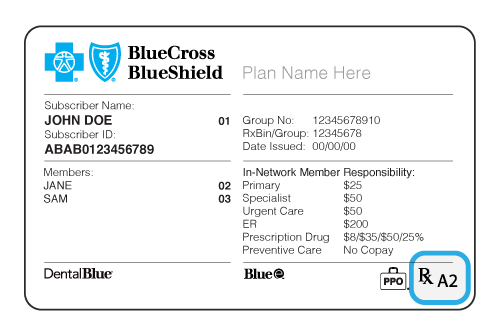
1) Look for the "Rx" on their fellow member ID bill of fare. Information technology means they take medication coverage.
2) Look for a majuscule or a capital letter/number combination afterwards the 'Rx' on your patient'south menu. The alphabetic character will tell you which drug list, or formulary, your patient'south plan uses. The number gives information most the pharmacies in your patient's network.
Enhanced Drug Listing
A, B,
Essential Drug List
C, D
Net Results Drug Listing
E
How to Find Your Patient'due south Canonical Medication List or Formulary
1) Return to the Providers homepage
- Click Discover Doctor / Drug / Facility on the top toolbar
ii) On the Observe a Doc, Drug or Facility page
- Click the Discover a Drug or Pharmacy tab
- Click Employer & Employee plans
- Respond Yes or No to the member ID bill of fare question
- Select the member's plan type from the card
- Click Run into Drug Coverage
You'll go to Prime Therapeutics, our pharmacy do good manager'southward website. Your patient'south medication list, or formulary, search should expect similar this:

three) Type a medication name in the blue search box, select the formulation and strength you are prescribing and click Submit.
- The medication name, description and cost tier info will appear below the search tool nether "Selected medicines." Additional details, such equally generic availability and pricing, are found under "See all pricing options."
- If you lot need to request prior authorization or there are other special requirements, those should be listed here, too. A comprehensive list of formulary medications and prior authorisation requirements are found under "Helpful documents," just click the pdf with the formulary proper noun.
Medications that Demand Prior Authorization
Some medications demand additional information, in writing, from you before Blueish Cross NC tin can decide if they will be covered. Our drug search tool shows the restricted medications our members use most, the requirements for approval, and the details you must send us to get them approved.
Enter a drug proper noun in the search box to encounter if it needs approval before it's covered by a patient's programme.
Or click the offset letter of your drug to view lists:
To find a drug, apply the search above or select a letter from the list above.
Make Drug Name: {{header}}
- Generic Drug Proper noun:
- Benefit: ,
- Specialty:
- Prior Review Required On: ,
MN Prior Authority: ,
- Quantity Limits Required On: ,
- Quantity Limits:
- Restricted Admission/Pace Therapy On: ,
- Restricted Access/Step Therapy:
- Nonformulary on: ,
- Nonformulary:
- Criteria: ,
- Fax Class: ,
- Note:
No results found for '{{header}}'
Prior Authorization
Providers must explicate in writing why patients need a certain medication before Blue Cross NC can decide if information technology will be covered.
Quantity Limits
To encourage the proper use of prescription medications, Blue Cross NC may restrict the amount of medicine an insurance plan covers. This may hateful taking fewer pills each day without changing the full strength of the medication.
Step Therapy
Bluish Cross NC requires that patients first attempt a medication or device that is not restricted before a restricted medication will be approved. Patients may exist covered for a restricted medication if providers tell Bluish Cantankerous NC in writing that:
The patient has already used the non-restricted medication and it wasn't constructive in treating the condition; or
The provider thinks the non-restricted medication is likely to exist harmful to the patient's health or not constructive in treating their condition.
Non-formulary
A non-formulary medication is 1 that isn't on a patient'south Blueish Cross NC medication list. Not all medication lists or formularies take not-formulary medications. Providers must confirm that a patient has tried the medication(s) on their list first, and that they were ineffective or harmful. Also, any medication-specific clinical criteria must be met earlier approval (available in the Drug Search).
Specialty Drugs
May be used to treat a complex or rare status, and are generally:
- Prescribed with special dosing or administration
- Prescribed by a specialist
- Significantly more expensive than culling therapies
Specialty drugs are express to a 30-day supply and patients must get them from an in-network specialty pharmacy, and so their benefits will use to the prescription. In-network pharmacy options vary based on the patient's plan benefits.
Important: If your patient has changed health plans, you may need to tell us that your patient has met the rules for their new programme.
For Patients with an Essential Medication List (Formulary): If your patient meets the Criteria for Approval of Restricted Products (pdf), and their list says that Prior Review (Prior Authorization) or Step Therapy is required for a medication, but the medication isn't in the Drug Search, delight send a request to Blue Cross NC using this General Dominance Fax Form (pdf).
Requesting Medications Not on Your Patient's Approved Medication List (Formulary)
For fastest processing, delight submit requests online using CoverMyMedsTM. If all details are submitted online and the asking is approved, the fellow member may be able to pick upwardly their prescriptions at the pharmacy in less than 2 hours.
Other processing methods include:
- Fax: 800-795-9403
- Postal service: Blue Cross NC, Attn: Corporate Pharmacy, PO Box 2291, Durham, NC 27707
Once we have all required information, we'll make a decision within iii business days and notify you. Requests are processed within 72 hours, unless urgent.
Urgent requests are handled inside 24 hours. An urgent asking is when you believe a delay would seriously jeopardize the life or health of the patient, the patient's power to regain maximum role, or would subject the patient to astringent pain that cannot be fairly managed without the care or treatment requested.
If you lot want your patient to take a medication that isn't on the Essential or Cyberspace Results medication list, here's what to practise:
- Consider if there'south another medication they could take.
- Check to see if the new medication is on the medication list. If it's there, y'all're all set!
- If you nonetheless need the non-formulary medication, send u.s.a. a request to approve the non-formulary medication.
- For approval, the patient must come across the Non-Formulary Exception Criteria (pdf). If the medication is listed in the Drug Search, these requirements may also apply.
- You must send all the details, with your signature, to Blue Cross NC.
- All requests tin can be submitted using CoverMyMeds or fax.
- If a medication is not listed in the Drug Search, request it using the Full general Authorization QL Fax Grade (pdf)
- If the medication is listed in the Drug Search, apply the fax grade shown there.
- For questions, or to check the status of your review, phone call us at 1-800-672-7897.
For members on the Essential Medication List (formulary), if request for a non-formulary medication is canonical, these cost levels or "tiers" will apply:
Essential 5 Tier = Tier v
Essential 6 Tier = Tier half dozen
For members on the Net Results Medication List (formulary), if the request for a non-formulary medication is canonical, these cost levels or "tiers" volition apply:
Non-specialty medication = Tier 4
Specialty medication = Tier 5
Medications with Express or No Plan Coverage
Some medications may not be covered by the patient'south program or may have a limited amount the patient tin can receive. The Table of Drugs with Limited or No Coverage shows a sample listing. Not all limited medications are listed.
For self-funded and ASO patients, yous may need to phone call Blue Cross NC Customer Service for medication limits that may use. If you lot are unsure if your patient'southward grouping is an underwritten or self-funded/ASO group, telephone call the customer service number listed on the dorsum of your patient'south member ID carte du jour.
| Drug Type | Drug Limits |
|---|---|
| Infertility Drugs | For groups that, in 2013, had a $5000 lifetime maximum and were able to carry this over due to updates to the Affordable Care Human action, this benefit will remain bachelor. Otherwise, the benefit is as follows (call Customer Service to confirm): Underwritten and Individual/Family plans:
*Requires prior authorization before being covered |
| Sexual Dysfunction Drugs Related to Organic Disease (due east.g., Cialis, Viagra, Caverject) | Underwritten and Individual / Family plans: Tadalafil (Cialis) two.5mg or 5mg: 30 tablets per 30 days 4 tablets or units per 30 days |
| Sexual Dysfunction Drugs Unrelated to Organic Illness | All: Non covered |
| Prenatal Vitamins | Express to members that are planning pregnancy, currently significant, or breastfeeding. If you believe you should qualify for an exception, please have your provider complete this form, and submit to Blue Cross NC for review. View the prenatal vitamin criteria for approval. In addition to the above benefit limitation, some prenatal vitamins are excluded from coverage entirely. These include, just are not limited to:
|
| Non-Food and Drug Administration (FDA) Approved Drugs | All: Not covered; please see the non-FDA approved medication and production list for specific medications that aren't covered |
| Initial fill of immediate-release opioid | All: Limited to maximum of vii days for initial fill. If this is non the kickoff fill, just Blue Cantankerous NC does not have the patient's claims history, utilise this IR Opioid QL Criteria (pdf) and IR Opioid QL Fax Course (pdf). |
| Prescription medications with over-the-counter (OTC) alternatives | Please encounter member guide for coverage. Not covered as a standard do good. Please see list for specific drugs that are non covered. |
| Medications used solely for weight loss | Please come across member guide for coverage. Non covered as a standard do good. Please encounter list for specific drugs that are not covered. |
| High Dollar Verification | Single claims over $10,000 require prior authorization (excluding antivirals, anti-infectives, anti-convulsants, insulin, specialty medications, and medications already subject to Prior Dominance or Pace Therapy requirements). Criteria data can exist plant hither, and fax submission information can be found by clicking here. |
Brand-Name Drugs vs. Generics
Don't let your patient over pay! They could be charged more if you prescribe a brand-name medication instead of a generic. If there'due south a medical reason the patient needs a brand-name medication, please:
- Check the Request for Waiver of Brand Drug Fees to see if your patient meets our requirements.
- Send a Safety MedWatch Form to the FDA tell them why your patient tin't take the generic.
- Transport us a Request for Waiver Faxback Form with your patient'southward details.
fitzgeraldnortur54.blogspot.com
Source: https://www.bluecrossnc.com/providers/medical-policies-and-coverage/prescription-drugs
0 Response to "Can You Please Tell Us Again Where to Find the Drug List Am Not Finding It Did You Say Bcbscom"
Post a Comment